

Welcome to the Narrative Patient Centered Care online module. This Module is presented in three parts:
I. Introduction to Narrative Patient Centered Care
II. Communication Skills for Narrative Patient Centered Care
III. Caring for the Whole Person and Family
In Part III, Caring for the Whole Person and Family, you will observe Wendy’s follow-up visit with her primary care provider and her partner, Oscar and explore the dimensions of whole person care, including spirituality.

". . . That business of the spirit, of the non-material self, of sympathy for and knowledge of others is the most important thing: in how we love, in how we live, and in what matters."
Colm Tóibín, writer and novelist
Each time patients who are seriously ill experience a medical incident they are confronted with their mortality and the associated issues of meaning and grief that are critical dimensions of the whole person experience.
Whole person care seeks to comprehend and address the physical, emotional, social, cultural and spiritual dimensions of the person to relieve suffering and promote healing.
Whole person care is focused on adapting to a changed life and draws on the inner resources of the patient and family with the patient in control. Whole person care complements biomedicine which is focused on preserving life.
Hutchinson T 2011

... it sounds trite, yet I can only say that I realized for the first time that I don't have forever....
In the first stages of my illness, I couldn't sleep, urinate or defecate - the word ordeal comes to mind. Then when my doctor changed all this and everything worked again, what a voluptuous pleasure it was. With a cry of joy I realized how marvelous it is simply to function. My body, which in the last decade or two had become a familiar, no longer thrilling old flame, was reborn as a brand-new infatuation.
I realize of course that this elation I feel is just a phase, just a rush of consciousness, a splash of perspective, a hot flash of ontological alertness. But I'll take it, I'll use it. I'll use everything I can while I wait for the next phase. Illness is primarily a drama and it should be possible to enjoy it as well as to suffer it. I see now why the romantics were so fond of illness - the sick man sees everything as metaphor. In this phase I'm infatuated with my cancer. It stinks of revelation.
As I look ahead, I feel like a man who has awakened from a long afternoon nap to find the evening stretched out before me. I'm reminded of D'Annunzio, the Italian poet, who said to a duchess he had just met at a party in Paris, ''Come, we will have a profound evening.'' Why not? I see the balance of my life - everything comes in images now - as a beautiful paisley shawl thrown over a grand piano....
Read the full essay in the New York Times
Think of a loved one or a patient with serious illness who you believe received good medical care that provided healing, even when medicine did not have a cure for their disease. What made their care “good”? How did you, or other clinicians provide healing? What were the signs that healing was happening?
Click on the button up to see what most patients and families say.
A. Doorenbos, pain module
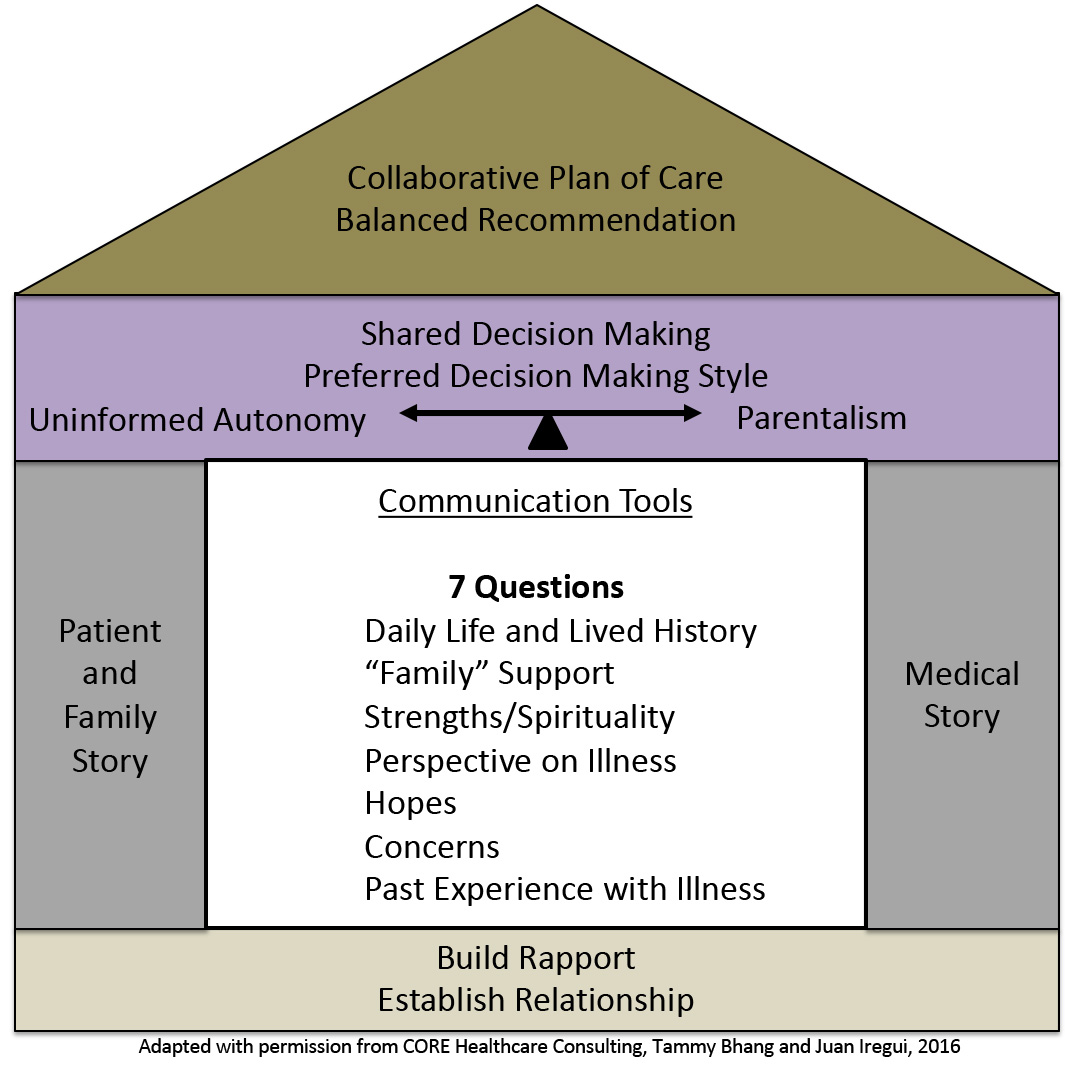
The 7 Questions presented in Part II will help you gain a deeper understanding of the whole patient and their family and ensures that the treatment you provide supports a meaningful life for everyone involved.

Lo, Ruston, Kates, et al. 2002
While Wendy’s nociceptive pain is controlled, she continues to describe a different kind of “pain” that doesn’t respond to her pain medications. It is a deep ache in her chest made worse when she thinks about what will happen to her grandchildren and her relationship with Oscar.
Treatment of nociceptive pain in cancer patients is a critical first step in addressing whole person pain. Continued support in dealing with the emotional, psychological, cultural and spiritual concerns of patients with advanced illness is also critical for treating the whole person’s pain.
At the end of the last visit the clinician asked Wendy if Oscar could participate in their next meeting in order to find out his perspective of the situation and to help the two of them work together.
Observe the differences in the attempts to set the context for the follow-up visit with Oscar and Wendy in the videos below. After watching each video, you will be asked to identify the communication skills you observed.
Quite a lot happens during the three-way discussion with Wendy, Oscar and the primary care provider. Use the check list below to identify the communication skills that that were most effective in this interaction.
With experience, you will adapt the skills for Narrative Patient Centered Care to your own style and modify them as the situation requires.
Think of them as individual tools in a toolbox, and as your skill develop you will be able to identify what tool works best for which situation.
As you will see, Wendy’s clinician uses some, but not all, of the Seven Questions as well as tools discussed in Part II.
You will also notice that Oscar answers some of the Seven Questions when a different Seven Question was asked.
Wendy’s clinician does not shy away from discussing Oscar’s spiritual beliefs. He acknowledges Oscar’s beliefs as important which demonstrates alignment with Oscar’s values, even if the clinician does not subscribe to the same values.
Observe the differences in the attempts to summarize and confirm Oscar’s story in the videos below. After watching each video, you will be asked to rate the clinician’s use of Narrative Patient Centered communication skills.
In Part III, Caring for the Whole Person and Family, you observed Wendy’s follow-up visit with Oscar and her primary care provider. You saw that managing Wendy’s whole person care included both nociceptive pain control and attention to the other important issues that were causing her distress.
The communication skills learned in Part III were used to deepen and extend the narrative approach during the follow-up visit, including spiritual concerns.
Part III allowed you to see how the 7 Questions can be helpful for both patients and their families, to deepen our understanding of their story and integrate the patient, family and medical narrative.

Hutchinson T. “Whole person care. In: Whole Person Care: A New Paradigm for the 21st Century. Hutchinson T, Ed. New York: Springer 2011.
Lo, Ruston, Kates, et al. Discussing Religious and Spiritual Issues at the End of life: A Practical Guide for Physicians. JAMA Feb 13, 2002-Vol 287, No. 6: 749754.