You are the receiving provider in the ICU for Mrs. Castillo. You received the transfer report, and know that she was found down at home by a friend and brought to the ED for further evaluation. Her past medical history is significant for hypertension (though she is currently hypotensive), type 2 DM, osteoporosis, hyperlipidemia, restless leg syndrome, and recent falls.

On arrival to the ED, she was found to have respiratory failure and was intubated. She received a bolus of 1 L of NS for hypotension in the ED. Radiologic exams were significant for a right acute on chronic subdural hematoma (SDH) without shift, and multiple old and new rib fractures. Her spine CT was negative. Neurosurgery has been consulted for the SDH and deemed she will not benefit from surgery at this time. She received fentanyl for pain. She has 2 adult children but they have not been reached at this time. Unclear if advance directives exist.


1Advanced trauma life support (ATLS®): the ninth edition. ATLS Subcommittee et al. J Trauma AcuteCare Surg. (2013).
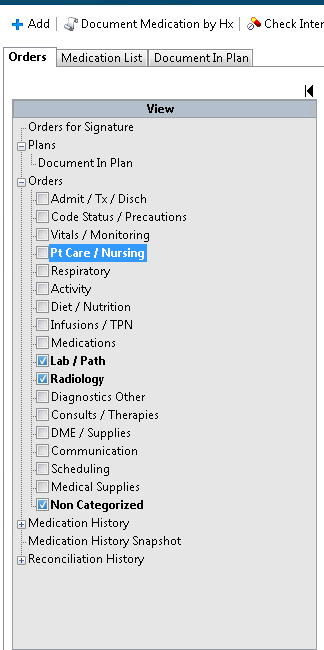
Admit to ICU
Dx: SDH, Hyponatremia, Respiratory Failure
As the Physician or Advanced Practice Provider reviewing the expert problem list, which nursing care, diet, and activity orders should be included in the admitting orders for Mrs. Castillo? Type your answer in the box below.



Current vital signs:
BP 92/48 mmHg; HR 122 BPM; RR 18 BPM; SpO2 97%

Check all the boxes that apply:



Your concerns over falls and rib fractures should trigger an evaluation of home safety, assessment of Mrs. Castillo’s capacity for continued independent living, and raise a concern for possible abuse and/or neglect. Social work, PT/OT, and other team members are appropriate to involve in these assessments. These consults should be ordered immediately because they directly impact the discharge plan and are critical to maintaining the patient’s safety both in and out of the hospital. These team members will gather as much information as possible from Mrs. Castillo, Mrs. Castillo’s family members and friends, medical records and other care providers.
Mrs. Castillo’s daughter, Angelina, arrives at the hospital.



Four hours after admission to the ICU, the team begins evening rounds. During the assessment they find Mrs. Castillo interactive and oriented to name and place, and following simple one-step commands. She is tolerating the ventilator. When asked if she is in pain, she gestures to her back and left side. She has been receiving pain medications every 1-2 hours with some relief, but remains restless with occasional facial grimacing.

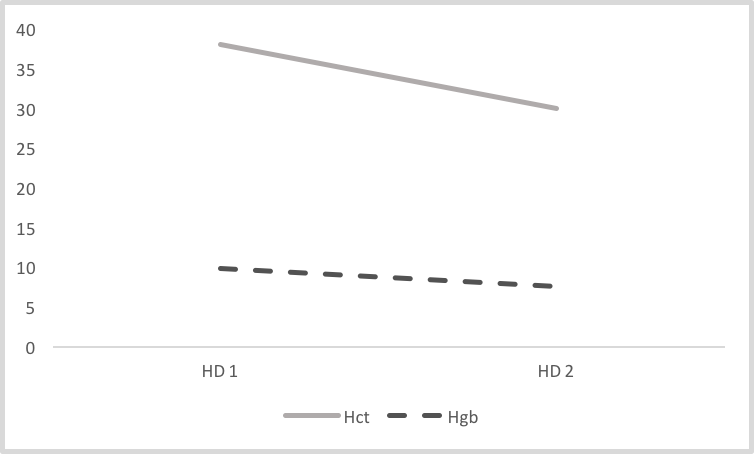

Hemorrhage should always be considered in the differential diagnosis. Systemic symptoms of bleeding would include changes in vital signs (tachycardia, hypotension) and pallor. However, Mrs. Castillo’s presentation does not match this presentation.
Family is updated on patient’s status/plans during morning multidisciplinary rounds.
Due to issues on Hospital Day 1 with pain control, an order was written to check with provider first before spontaneous breathing trial (SBT). You are now approached by the respiratory therapist who asks if there is any reason why a SBT should not be attempted with Mrs. Castillo.
Following a successful SBT, Mrs. Castillo was able to be extubated.
Following extubation, she is alert and oriented X3, but has deficits in short-term memory. She was ambulated OOB to chair, but was easily fatigued. The social worker interviews the patient, and the family is determined to be safe and supportive. Mrs. Castillo confirms that her goal is to continue living independently. Therefore, she will need to maintain and regain optimal function.

Mrs. Castillo is stable overnight and plans are made to transfer her to the hospitalist service and the medicine acute care floor.
The following areas of information are included in the transfer note. Use the box below to write the areas of information that are missing from the note.
Following her transfer to the medicine floor, Mrs. Castillo continued to stabilize medically. Physical therapy continued to work with Mrs. Castillo regarding mobility, balance and conditioning. In addition, speech therapy was started to assist with cognitive strategies. Mrs. Castillo was ultimately discharged to rehabilitation for continued therapy.
You have now completed the case study.
Please click on the link below to provide feedback on your experience.

Coffin SE, et al. Strategies to prevent ventilator-associated pneumonia in acute care hospitals. Infect Control Hosp Epidemiol 2008 Oct;29 Suppl 1:S31-40.
AACN Practice Alert - Ventilator Associated
Pneumonia:
Gould CV, et al. Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for prevention of catheter-associated urinary tract infections 2009. Atlanta (GA): Centers for Disease Control and Prevention (CDC); 2009.
Marschall J, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infect Control Hosp Epidemiol 2008 Oct;29 Suppl 1:S22-30.
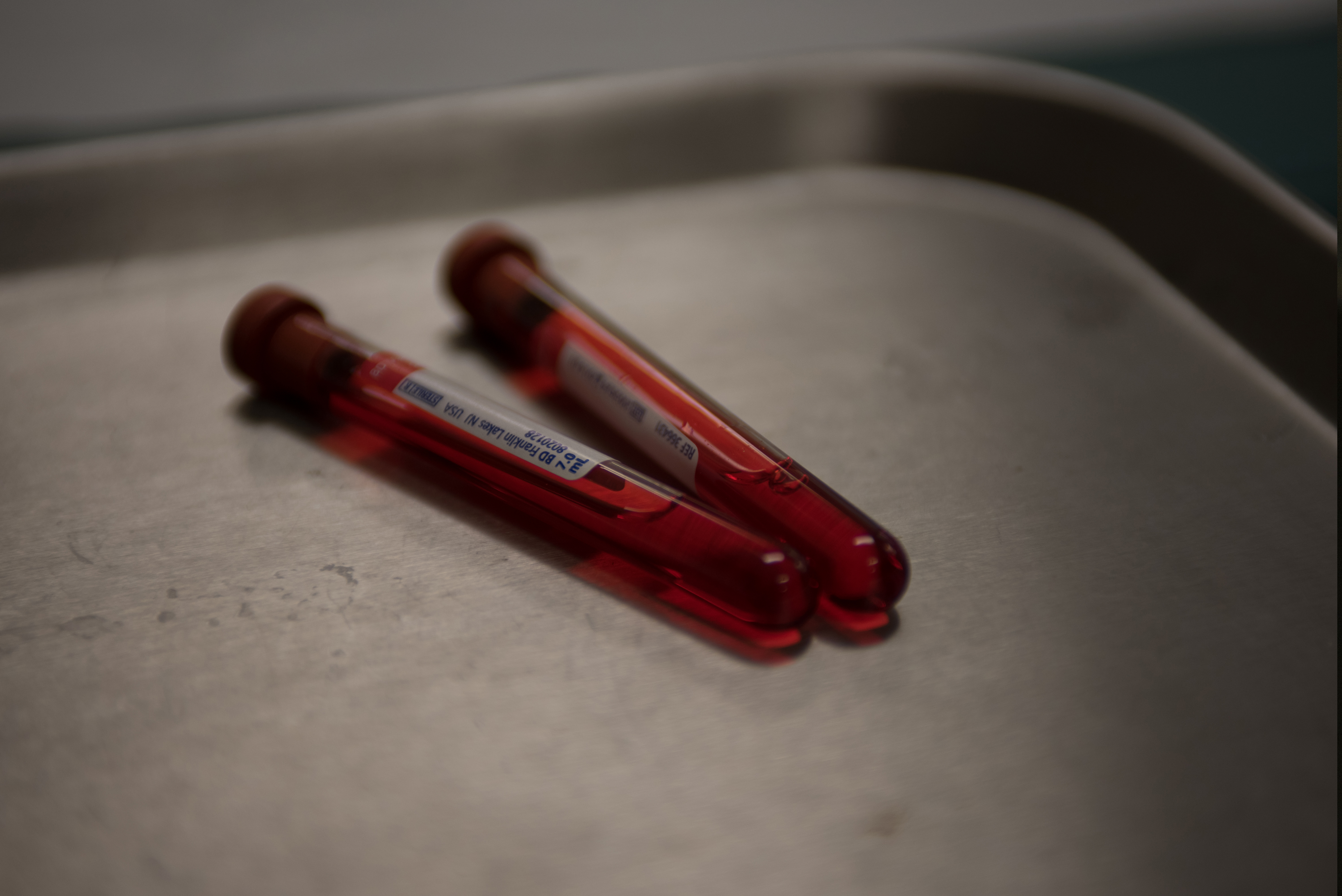
Blood Alcohol Level: 0
INR: 1.0 (normal)
PTT: 35 seconds
CBC:
Hgb 9.9 g/dL
Hct 38%
RBCs 4.4 x 106 cells/mcL
Platelets 152,000/mm3
WBC 12,000 cells/mcL
Neutrophils 70% - Hi
Lymphocytes 23%
Monocytes 6%
Eosinophils 1%
Basophils 0.2%
BMP:
BUN 27 mg/dL
CO2 22 mmol/L
Creatinine 0.95 mg/dL
BUN/Creatinine Ratio: 28 - Hi
Glucose 310 mg/dL - Hi
Sodium 112 mEq/L - Lo
Chloride 85 mEq/L
Potassium 4.3 mmol/L
GFR calculated: 57.7 mL/min/1.73 m2 - Lo
Troponin: 0.01 ng/mL negative
CK: 50 U/L
U/A- wnl, except for + protein
Urine Toxicology Screen-negative
Serum Na+, Serum Osmolality, Urine specific gravity, Urine Na+, Urine Osmolality
Multiple left-sided rib fractures. Most of these appear to be chronic and healed; however, there are acute-subacute appearing fractures of the anterolateral aspect of the left 4th and 5th ribs. Ununited chronic fracture of the lateral aspect of the left 6th rib.
Spine CT: No fractures.
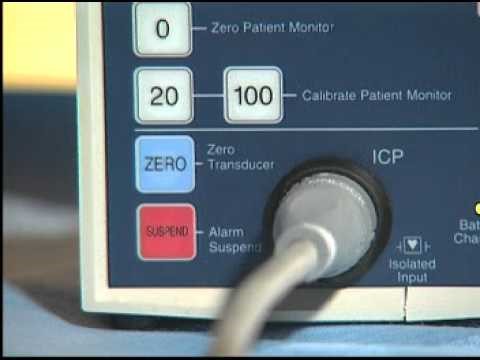
Head CT: 3mm right acute on chronic holohemispheric subdural hematoma without shift. No noted skull fractures.

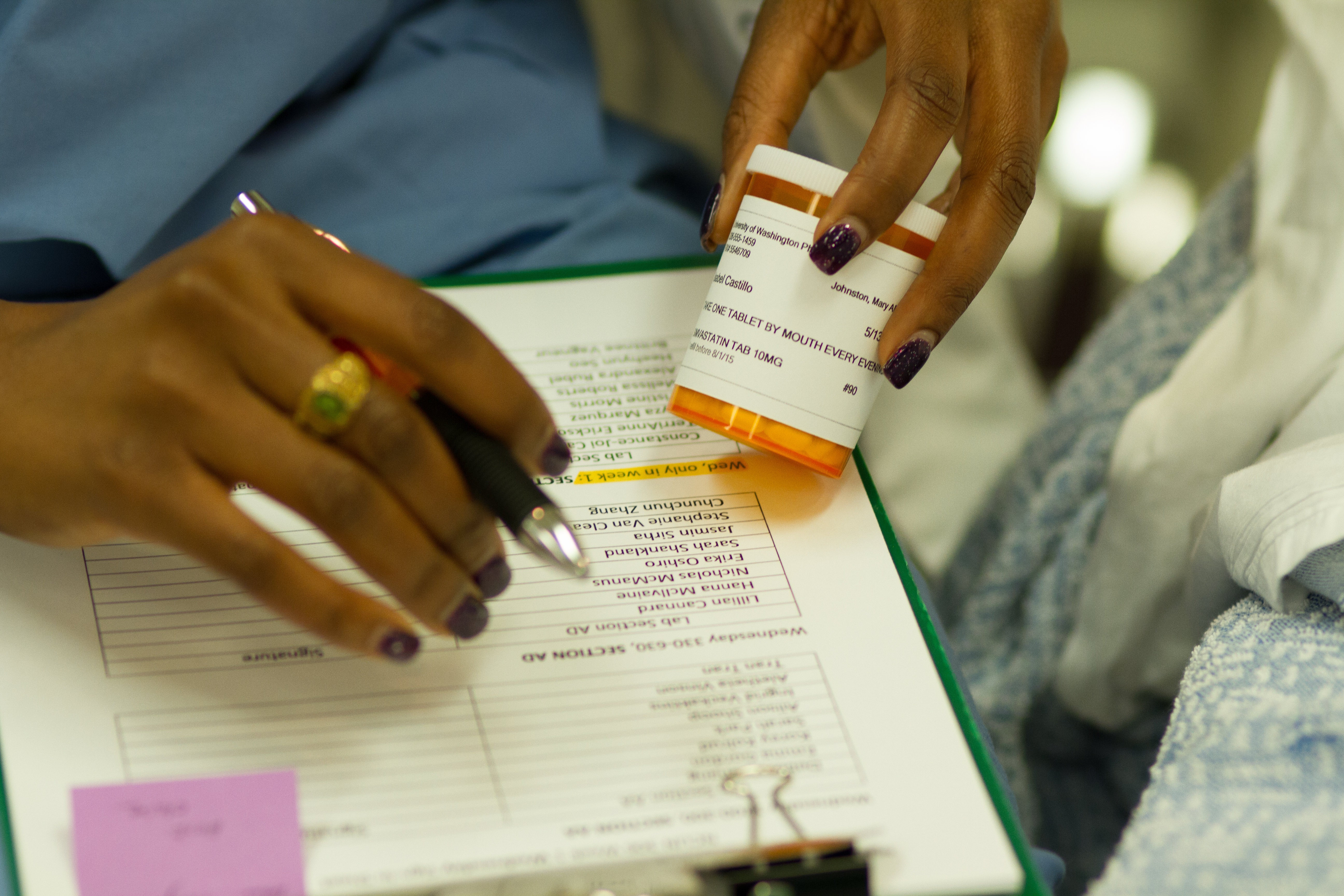
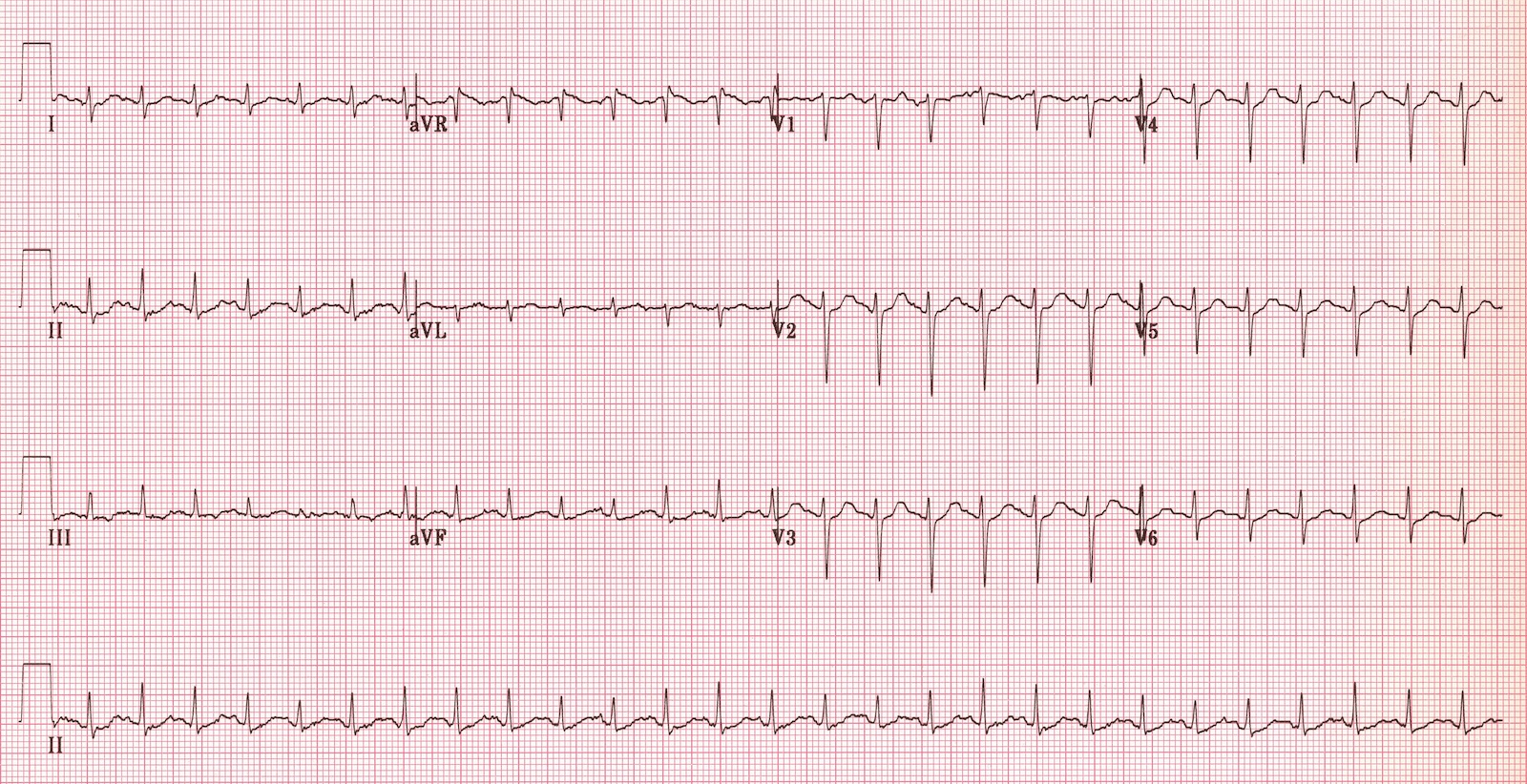
Photo courtesy of UW Medicine.

Aspirin therapy, such as Mrs. Castillo was receiving, disrupts platelet function by inhibiting COX1 for the life of the platelet (~7-10 days). Presently, platelet transfusion for patients receiving antiplatelet agents, such as aspirin, is controversial and requires further study. A summary of work in this area is provided in the link below.