You are the acute care provider assigned to care for Mr. Miguel Sanchez in the ICU of Sleepy Valley Hospital, which is a 60-bed hospital located in rural Washington State.
Mr. Sanchez was brought to the Sleepy Valley Emergency Department (ED) at 9:00 am by his wife, Rosa. He is a 54-year-old Hispanic male who presented to the ED with shortness of breath (SOB), fatigue, and bilateral lower extremity swelling. His diagnosis in the ED was acute decompensated heart failure (ADHF). As you review his ED records you note the following:

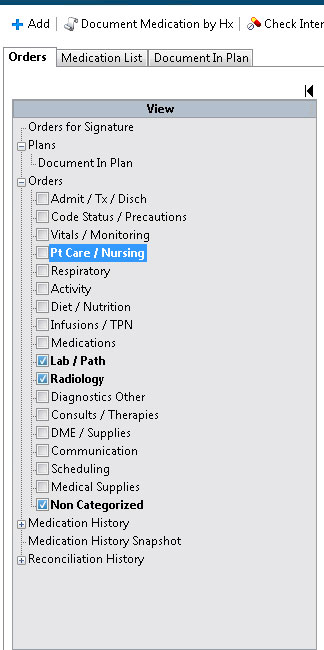
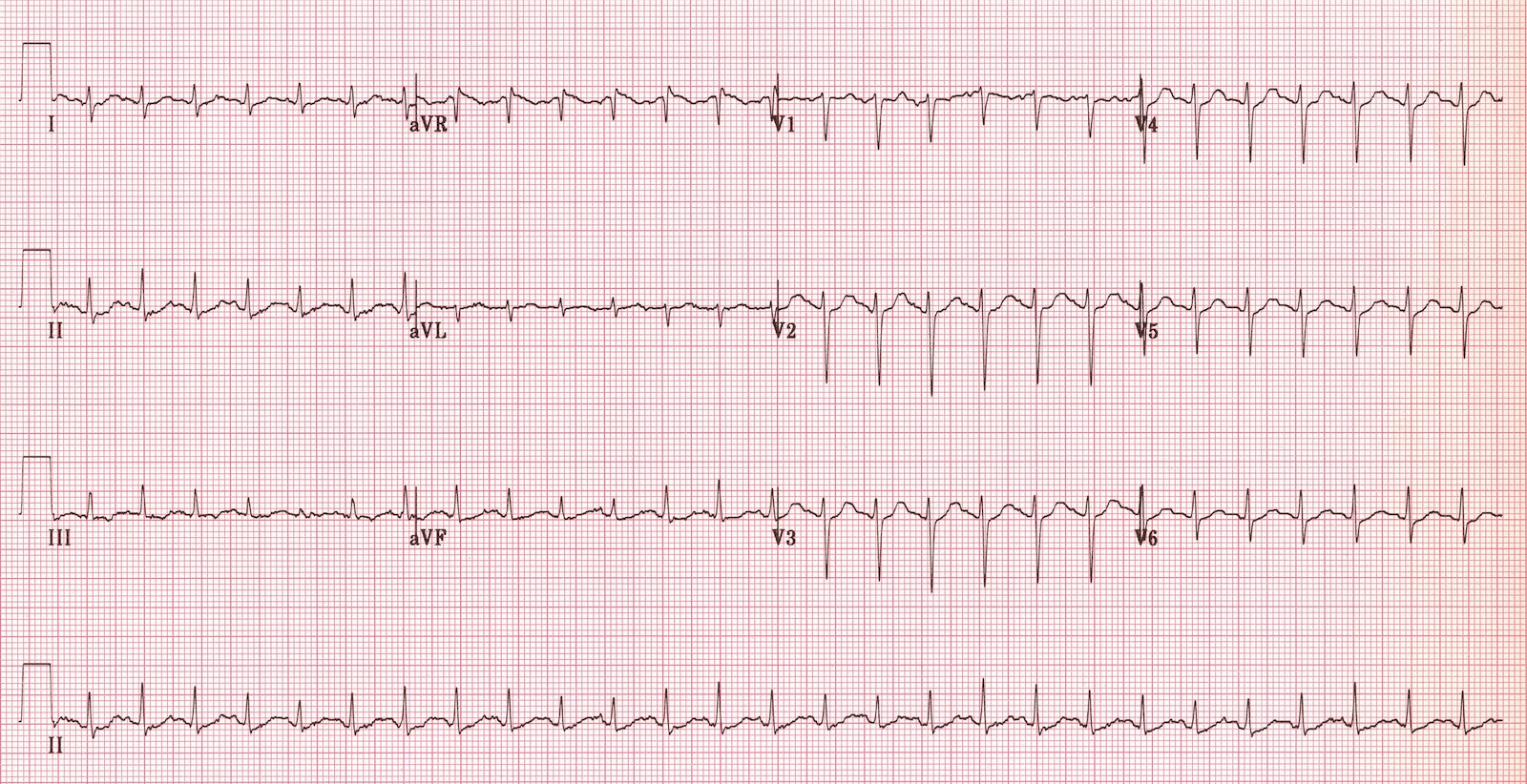
You know from the handoff phone call from the emergency physician that Mr. Sanchez was examined in the ED and placed on supplemental oxygen therapy at 2 L/minute via nasal cannula and an intravenous (IV) catheter was inserted into his left arm. Blood work was ordered for comprehensive metabolic panel (CMP) and complete blood count (CBC) and urinalysis (UA) was sent to the lab. An electrocardiogram (ECG)and a chest x-ray (CXR)were completed. He was given 40 mg of furosemide IV and admitted to the ICU.
Mr. Sanchez has just arrived in the ICU. The bedside nurse is placing Mr. Sanchez on a cardiac monitor. You enter the room to begin your assessment and overhear his wife, Rosa, telling the nurse that “this is the second time in 6 months he has been in the hospital for this problem.”
Please drag the bottom right corner to expand the box.

Mr. Sanchez might not have met criteria for ICU admission in all hospitals. It is important to be aware of ICU admission criteria for your individual institution. Institutions vary on ICU admission criteria regarding patient status, diagnosis, and prognosis, capability to provide specific treatments, available clinical expertise, nurse staffing to patient ratios, and bed availability.
Nates, J. L., Nunnally, M., Kleinpell, R., Blosser, S., Goldner, J. et al. (2016). ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Critical Care Medicine, 44(8), 1553-1602. doi: 10.1097/CCM. 0000000000001856
Yancy, CW, Jessup, M, Bozkurt, B, Butler, J, Casey, DE, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 128:e240-e327. doi: org/10.1161/CIR.0b013e31829e8807
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(3). DOI: 10.1161/CIR.0000000000000509.

While being treated in the ED and ICU, the main medical providers involved in Mr. Sanchez’ care are the acute care provider,cardiologist, and pharmacist. Please click on each of the boxes below to see what the roles are for each provider.
Yancy, et al. 2013 ACCF/AHA guideline for the management of heart failure. doi: org/10.1161/CIR.0b013e31829e8807

Even though Mr. and Mrs. Sanchez speak some English, Mr. Sanchez has stated that he prefers to have his medical team talk to them in Spanish. As the provider, you have limited conversational Spanish.


You access Sleepy Valley’s on-demand video interpretation service because there is no in-person interpreter available and conduct Mr. Sanchez’ history.
Click on the recording below to listen to a portion of the conversation between the patient and provider, facilitated by the interpreter, to assess his heart failure symptoms.

A summary of Mr. Sanchez’ history is below. Click on each heading to see the related information.
Click on the headings below to show more information.
Reports shortness of breath for 3 days, increasing in severity to the point he is unable to perform his normal exercise routine and is limited to walking to the front door of his house only. Reports eating salty foods during a recent family party. Reports bilateral lower extremity swelling for the past few days. He reports around a 7-pound weight gain over the past 24-48 hours. His wife reports he has been lying in bed all day, which is not normal for Mr. Sanchez; he is normally quite active. He reports his last echocardiogram (echo) was approximately 6 months ago when he was in the hospital. He recalls being told his heart function was not normal. His wife says she thought he needed to be seen because he has become SOB while sitting in the chair watching TV.
+ SOB, dyspnea, orthopnea (3 pillows), & PND. Decreased appetite X 2 days. + weight gain. No fever, chills, nausea/vomiting or chest pain or other pain. No dizziness or lightheadedness. No cough or sputum production. No dysuria.
Coronary artery disease (CAD) s/p myocardial infarction (MI), s/p coronary artery bypass graft surgery (CABG), HF (diagnosed 2 years ago), hypertension, and hyperlipidemia. Last hospitalized for heart failure exacerbation 6 months ago, ejection fraction was 45% on cardiac echo, creatinine was 1.2 milligrams (mg)/deciliter (dL).
CABG 2 years ago, cardiac catheterization also 2 years ago (before surgery); laparoscopic cholecystectomy 2001, tonsillectomy (child).
Former cigarette smoker, quit 2 years ago (36 pack-year history). Employed as a job construction manager, enjoys yardwork, fishing, exercises 2-3 times/week (walking in his neighborhood with his wife). Married to wife, Rosa, for 20 years; they live together nearby. They have 2 adult children. Drinks alcohol socially (1-2x per week approx. 2 beers in 1 day when drinking) and no history of substance abuse.
Recent changes: unable to participate in yardwork, hobbies or exercise.
CAD (father), hypertension (father, mother, paternal grandfather), hyperlipidemia (father, mother, paternal grandfather), Type 2 diabetes (mother), breast cancer (maternal grandmother).
No known drug, food or chemical allergies.
 Aspirin 81 mg orally daily
Aspirin 81 mg orally daily
Furosemide 20 mg orally twice daily
Potassium chloride 10 milliequivalents (mEq) orally daily
Lisinopril 10 mg orally daily
Rosuvastatin 20 mg orally at bedtime
Ibuprofen 400 mg orally 3-5 times/day, has been taking for approximately 6 months for knee pain.
Metoprolol succinate 25 mg orally daily has been prescribed, but he reports he stopped taking it because “it made me too tired.”
Signs and symptoms of acute decompensated heart failure aid the provider in classifying heart failure with either the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) Stages of Heart Failure or the New York Heart Association (NYHA) Functional Classification. The ACCF/AHA classification is progressive and patients do not move back and forth between stages. Patients can move back and forth between the NYHA classes depending on their symptoms at any time. The ACCF/AHA classification is progressive and patients do not move back and forth between stages. It is helpful to use both classification systems since they have different functions.
A quick, noninvasive technique to evaluate a patient’s hemodynamic status is by assessing for congestion (“dry” versus “wet”) and adequate peripheral perfusion (“warm” versus “cool”). This categorization can be helpful in guiding management decisions.
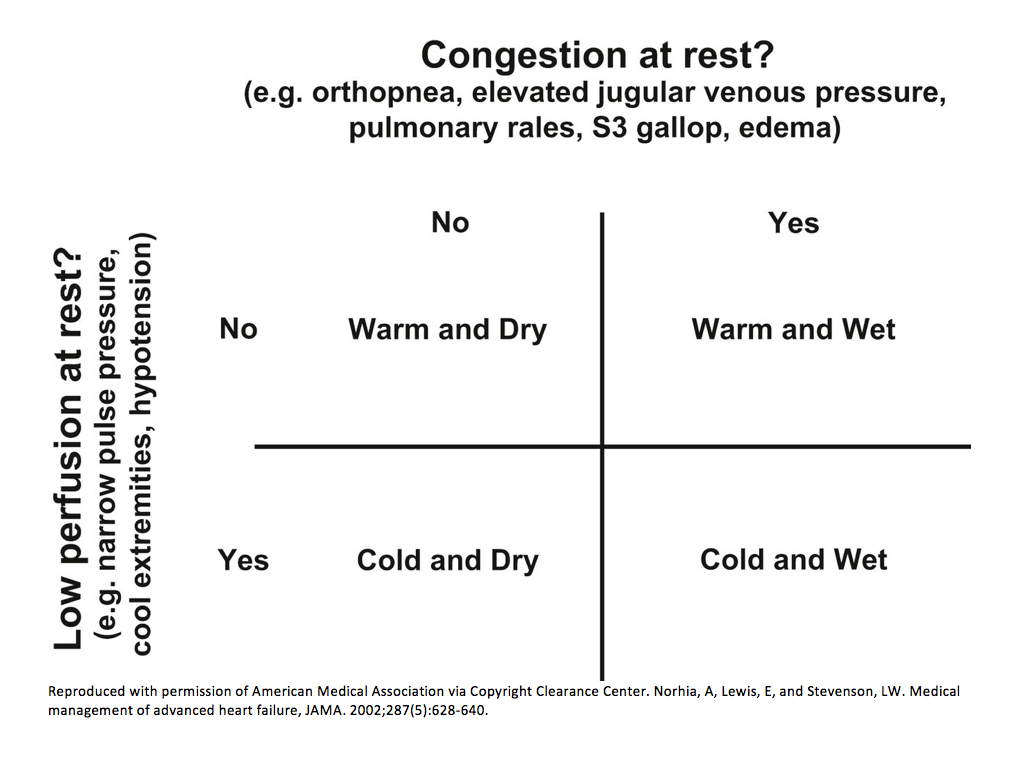
Nohria, A., Tsang, S. W., Fang, J. C., Lewis, E. F., Jarcho, J. A., Mudge, G. H., & Stevenson, L. W. (2003). Clinical assessment identifies hemodynamic profiles that predict outcomes in patients admitted with heart failure. Heart Failure, 41(10), doi: 10.1016/S0735-1097(03)00309-7
A patient with a history of heart failure requires a comprehensive physical examination.
What physical exam information should be gathered on admission?
Please drag the bottom right corner to expand the box.

Click on the headings below to show more information.
BP, HR, RR, temperature, height, weight, BMI and SpO2
Bickley, L. S. (2017). Bates’ Guide to Physical Examination and History Taking (12th ed.). Philadelphia: Wolters Kluwer.
A physical exam of Mr. Sanchez reveals the following findings most pertinent to his current condition.
Click on each heading below to see more information.
T 37.1° C, HR 104 bpm, BP 104/62 mmHg, RR 24 bpm, SpO2 96% on 2L nasal cannula
Trachea midline. Carotid pulses 2+ bilaterally, without bruits. JVD is at the angle of the jaw.
S1S2 heart sounds and S3 is present at the apex. No murmurs. Regular rate. PMI is diffuse, 3 cm in diameter, palpated at the anterior axillary line in the 5th and 6th intercostal spaces.
Thorax symmetrical. Anterior/posterior (AP) < lateral diameter. Equal expansion bilaterally. Respirations slightly labored. Bibasilar crackles at the bases. No rhonchi or wheezes.
Round. Bowel sounds normoactive. Soft without tenderness or masses. No hepatosplenomegaly.
+ tenderness and crepitus with movement right knee. No warmth or masses. Decreased active/passive ROM right knee.
Warm, dry, no clubbing or cyanosis of lips or nailbeds 3+ edema bilateral lower extremities (ankles to shins). 2+ Bilateral radial, dorsalis pedis (DP)/posterior tibial (PT) pulses.
Results from labs obtained in ED are now available. Click on each of the boxes below to see the results.
Click here to see normal ranges

White blood cell count (WBC) 5,800 cells/microliter (mcL)
Red blood cell count (RBC) 5.9 million cells/mcL
Hematocrit 32.7%
Hemoglobin 10.4 grams/deciliter (g/dL)
Mean corpuscular volume (MCV) 88 femtoliter/cell
Mean corpuscular hemoglobin (MCH) 28 picograms/cell (pg/cell)
Mean corpuscular hemoglobin concentration (MCHC) 35 g/dL
Platelets 254,000/mcL
 Sodium 131 milliequivalents/liter (mEq/L)
Sodium 131 milliequivalents/liter (mEq/L)
Potassium 4.9 mEq/L
BUN 21 milligrams/deciliter (mg/dL)
Creatinine 1.7 mg/dL
Glucose 95 mg/dL
Chloride 99 mEq/L
CO2 29 mEq/L
Calcium 10.0 mg/dL
Albumin 3.1 g/dL
Alkaline phosphatase 108 units/liter (U/L)
ALT 38 U/L
AST 20 U/L
Total bilirubin 1.5 mg/dL
Total protein 7.1 g/dL
Pending
Sinus tachycardia HR 110 bpm

Cardiomegaly, interstitial pulmonary edema with Kerley B lines

Click here for link for calculator
Please drag the bottom right corner to expand the box.

ACCF/AHA guidelines do not recommend routine invasive hemodynamic monitoring for ADHF patients who have a normal blood pressure. Hemodynamic monitoring via pulmonary artery catheter would not typically be recommended for Mr. Sanchez because he is not showing signs/symptoms of respiratory distress or impaired perfusion. It is important to assess patients clinically before more invasive monitoring is ordered.
Yancy et al. 2013 ACCF/AHA guideline for the management of heart failure. doi: org/10.1161/CIR.0b013e31829e8807
Please drag the bottom right corner to expand the box.

Please drag the bottom right corner to expand the box.


The IV loop diuretic dose started in the acute care setting for ADHF should be greater than or equal to the patient’s home dose of oral loop diuretic. The intravenous dose should be titrated to relieve symptoms of fluid overload, while remaining normotensive and not worsening renal function. Studies comparing continuous IV loop diuretics versus intermittent or bolus IV dosing of loop diuretics have shown mixed results. Most authors conclude that continuous IV loop diuretic therapy resulted in more efficient diuresis and reductions in BNP levels during hospitalization. However, authors from a recent meta-analysis (2014) concluded there were no significant differences in efficacy and safety with continuous IV loop diuretic therapy when compared with IV intermittent loop diuretic therapy in patients with ADHF.
Wu MY, Chang NC, Su CL, Hsu YH, Chen TW, Lin YF, Wu CH, Tam KW. Loop diuretic strategies in patients with acute decompensated heart failure: a meta-analysis of randomized controlled trials. J Crit Care. 2014 Feb;29(1):2-9. doi: 10.1016/j.jcrc.2013.10.009.
Yancy, et al. 2013 ACCF/AHA guideline for the management of heart failure. doi: org/10.1161/CIR.0b013e31829e8807
Patients admitted for ADHF are at increased risk for venous thromboembolism (VTE).
Which of the following would be appropriate pharmacologic intervention(s) for VTE prophylaxis? Choose all that apply.

Clinical practice guidelines recommend assessing all patients for VTE risk at hospital admission, change in level of care, and prior to discharge. Risk factors for VTE with ADHF patients may include: reduced cardiac output, left ventricular dysfunction, dilatation of cardiac chambers, increased central venous pressure, reduced myocardial contractility, endothelial dysfunction, platelet dysfunction, advanced age, obesity, and implantable cardiac defibrillator and/or pacemaker leads. Furthermore, patients admitted to the hospital with ADHF have an increased risk due to possible central venous catheters, acute medical illness, impaired mobility, and renal insufficiency. Prior to initiating VTE prophylaxis, clinicians should assess current renal status and the risks/benefits for each patient.
National Guideline Clearinghouse (NGC). Guideline summary: Venous thromboembolism prophylaxis. In: National Guideline Clearinghouse (NGC) [Web site]. Rockville (MD): Agency for Healthcare Research and Quality (AHRQ); 2012 Nov 01. [cited 2016 Dec 21]. Available: https://www.guideline.gov
Patient and family education is a continuous process for all patients, especially patients hospitalized who are receiving new treatments.
Patient education, early follow-up and multidisciplinary disease management have been shown to reduce readmission for heart failure exacerbation. Patient and family/caregiver education should begin early and continue throughout hospitalization. Social workers can assist with patient and family engagement in education and can be consulted early on during hospital stay to assist with providing culturally tailored education.
It is best to provide verbal and written instructions, especially regarding medications, to patients. Follow up appointments should be made prior to discharge from the hospital and communicated to the patient and caregiver in written format.
Discharge medication education should include new medications added while hospitalized and when last doses taken in the hospital. It is also important to discuss the patient’s previous medications (prior to hospitalization) to discuss if continuing, discontinuing, or dose was adjusted.
It is important to provide materials in the patient’s native language to improve the chance of compliance with the recommended treatment and optimize clinical outcomes. Click here to see resources for health information in multiple languages.
Albert NM, Barnason S, Deswal A, et al. Transitions of care in heart failure: A scientific statement from the American Heart Association. Circ Heart Fail. 2015 Mar;8(2):384-409. doi:10.1161/HHF.0000000000000006.
Wiggins BS, Rodgers JE, DiDomenico RJ, Cook AM, Page RL 2nd. Discharge
counseling for patients with heart failure or myocardial infarction: A best
practices model developed by members of the American College of Clinical
Pharmacy's Cardiology Practice and Research Network based on the Hospital to Home
(H2H) Initiative. Pharmacotherapy. 2013 May;33(5):558-80. doi: 10.1002/phar.1231.
Click here for medications that may cause or exacerbate HF (Table 1).
Click here to read the latest guidelines on managing ADHF.

Healthcare guidelines are documents that are written by specialty organizations about diagnostic criteria and management about specific illnesses based on systematic reviews of existing literature and evidence. Guidelines are intended to provide clinical recommendations. While clinicians should consider guidelines when choosing treatment options, they must make decisions based on the risk/benefit analysis for each patient.
Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines; Graham R, Mancher M, Miller Wolman D, et al., editors. Clinical Practice Guidelines We Can Trust. Washington (DC): National Academies Press (US); 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK209539/doi: 10.17226/13058
ACCF/AHA Guidelines recommend HF be treated with guideline-directed medical therapy (GDMT).
The pharmacist conducts the medication reconciliation and notes the following:
Aspirin 81 mg orally daily
Furosemide 20 mg orally twice daily
Potassium chloride 10 mEq orally daily
Lisinopril 10 mg orally daily
Rosuvastatin 20 mg orally at bedtime
Ibuprofen 400 mg orally 3-5 times/day for approximately 6 months
Spider milk weed, garlic
Metoprolol succinate 25mg orally daily, but he reports not taking it because “it made me too tired.”
Please drag the bottom right corner to expand the box.

In a 2006 study, approximately 80% of Hispanic patients (N=620) in an American urban health center responded to a survey of using herbal products. Most participants were unaware of the English name for the herb and did not report herbal use to their providers. This study highlights the importance of assessing herbal product use in the appropriate language. However, authors from a recent systematic review (2013), examined herb use among racial and ethnic minorities in the United States. The authors noted that herb use among Hispanics ranged from 4% to 100%, with a mean of 30%. They also found that Hispanics, as well as Asian Americans are less likely to inform providers about their herb use.
A useful resource is How Safe Is This Product or Practice?from the National Center for Complementary and Integrative Health which lists safety and efficacy information for Complementary, Alternative or Integrative Health (links to https://nccih.nih.gov/health/decisions)practices.
Gardiner P, Whelan J, White LF, Filippelli AC, Bharmal N, Kaptchuk TJ. A systematic review of the prevalence of herb usage among racial/ethnic minorities in the United States. J Immigr Minor Health. 2013 Aug;15(4):817-28. doi:10.1007/s10903-012-9661-z
Howell L, Kochhar K, Saywell R Jr, Zollinger T, Koehler J, Mandzuk C, Sutton
B, Sevilla-Martir J, Allen D. Use of herbal remedies by Hispanic patients: Do
they inform their physician? J Am Board Fam Med. 2006 Nov-Dec;19(6):566-78.
During the night, Mr. Sanchez was diuresed effectively and he was negative 3 liters in the past 24 hours. On this morning’s exam, his lung sounds are clear to auscultation bilaterally. Heart sounds are S1/S2 with no murmur, rub, or S3. The cardiac monitor shows normal sinus rhythm (NSR) with HR 87 bpm. His blood pressure is 110/72. His morning weight is 119.7 kg (3 kg weight loss). The 2-dimensional echocardiogram results show systolic HF with an ejection fraction (EF) of 40%.
Based on the above data, Mr. Sanchez is classified as “improved” and no longer meets criteria for the ICU. As the provider, you place orders for transfer to the medical floor with telemetry as well as physical therapy (PT) for progressive mobility. At time of medication reconciliation, IV diuretics are discontinued and Mr. Sanchez is transitioned to oral route of diuretic therapy. Low dose metoprolol is ordered to start this evening.

Additionally, patient prognosis and available resources of the institution (nursing staffing, etc) may play a role in the transfer.
Nates JL, Nunnally M, Kleinpell R. ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016 Aug;44(8):1553-602. doi: 0.1097/CCM.0000000000001856.
Please listen to the conversation and suggest how improve it.
Please listen to the conversation below and suggest how improve it.
Please drag the bottom right corner to expand the box.
Please drag the bottom right corner to expand the box.

McNeely EB. Treatment considerations and the role of the clinical pharmacist throughout transitions of care for patients with acute heart failure. J Pharm Pract. 2016 Apr 28. doi: 10.1177/0897190016645435

The registered nurse’s (RN’s) role is to work in collaboration with other health providers to anticipate and meet the needs of the patient and family facing serious and/or life-limiting illness. S/he also provides psychosocial, spiritual and culturally-sensitive support.
The role of the spiritual care provider is to offer culturally sensitive emotional and spiritual support to patients, families, and staff.
The priority for the spiritual care provider at this time is to:
The role of the dietitian is to assess a patient’s nutritional status, take anthropometric measurements to assess muscle stores, and provide nutrition recommendations to the team.
The priority for the dietitian is to assure the patient has:
Additionally, the dietician will:
The role of the nephrologist is to assist the care team in diagnosing and managing kidney disease.
Due to Mr. Brown’s condition, the priority for the nephrologist is to:
The role of the gastroenterologist is to assist the care team in symptom management of end-stage liver disease and lead discussions regarding lifesaving therapies (i.e., liver transplantation).
The priority for the gastroenterologist is to:

In many serious chronic illnesses, curative therapies such as transplantation exist, but patients have to be “sick enough to die,” but not “too sick” to be accepted onto a transplant list. In addition, many people have misinformation about what is required to be accepted onto a transplant list. Practitioners must ensure patients receive high quality therapeutic interventions while paying attention to evolving patient and family goals and values. Identifying deteriorating health status early and talking with the patient and family about the status is key to supporting them to make the most informed decision, even if that is not the decision a provider would recommend.
Pai, R., Karvellas, C.J. Is palliative care appropriate in a liver transplant candidate? Clinical Liver Disease, 6(1), 2015.
The role of palliative care is to help patients and their families explore and articulate their goals of care, and to ensure the patient's goals of care are factored into the healthcare team’s plan.
The priority for palliative care is to:

In institutions where there is a palliative care team, they often handle these discussions. However, there are many institutions that do not have a palliative care service. In that case, these tasks are completed by the providers caring for the patient. Some providers embrace the concept that palliative care is everyone’s responsibility, and will engage with patient and family around this topic, while others may not. It is important that the health care team have an open discussion about which members will participate in the discussion, who will lead the discussion, and when this discussion will take place.
Manages care for an acute illness or injury, typically for a short duration while in a hospital setting. Depending on the setting, this may be a Physician, a Nurse Practitioner, or a Physician Assistant. Additionally, the acute care provider discusses and negotiates the plan of care with the patient and family.
Blood Alcohol Level: 0
INR: 1.0 (normal)
PTT: 35 seconds
CBC:
Hgb 9.9 g/dL
Hct 38%
Platelets 152,000/mm3
WBC 12,000 cells/mcL
Neutrophils 70% - Hi
Lymphocytes 23%
Monocytes 6%
Eosinophils 1%
Basophils 0.2%
BMP:
BUN 27 mg/dL
CO2 22 mmol/L
Creatinine 0.95 mg/dL
BUN/Creatinine Ratio: 28 - Hi
Glucose 310 mg/dL - Hi
Sodium 112 mEq/L - Lo
Chloride 85 mEq/L
Potassium 4.3 mmol/L
GFR calculated: 57.7 mL/min/1.73 m2 - Lo
Troponin: 0.01 ng/mL negative
CK: 50 U/L
U/A- wnl, except for + protein
Urine Toxicology Screen-negative

Multiple left-sided rib fractures. Most of these appear to be chronic and healed; however, there are acute-subacute appearing fractures of the anterolateral aspect of the left 4th and 5th ribs. Ununited chronic fracture of the lateral aspect of the left 6th rib.
Spine CT: No fractures.
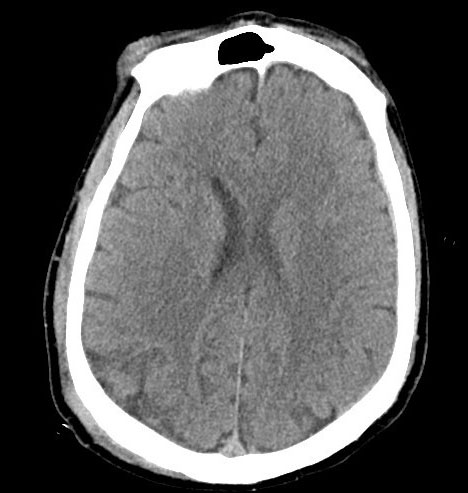
Head CT: 3mm right acute on chronic holohemispheric subdural hematoma without shift. No noted skull fractures.

Photo courtesy of UW Medicine.
The rationale for obtaining this consult is the presence of multiple rib fractures; need for assessment of possible elder abuse and locating legal next of kin (LNOK).
Social worker reports that she has attempted to contact patient’s daughter, but has not been able to reach her. Social worker will continue to reach out to daughter and locate other family members. Once family has been reached, social worker will conduct safety assessment for Mrs. Castillo, including assessing for possible elder abuse or neglect due to rib fractures.
The rationale for obtaining this consult is for surgical evaluation of the patient’s subdural hematoma.
Neurosurgery finds that the SDH is non-operable and recommends the transfusion of a 6-pack of platelets.

Aspirin therapy, such as Mrs. Castillo was receiving, disrupts platelet function by inhibiting COX-1 for the life of the platelet (~7-10 days). Presently, platelet transfusion for patients receiving antiplatelet agents, such as aspirin, is controversial and requires further study. A summary of work in this area is provided in the link below.
